Elbow Disorders Palm Beach County
(561) 746-7686
1002 S Old Dixie Hwy Jupiter, FL 33458
Monday - Thursday | 8:00 AM - 5:00 PM
Friday | 8:00 AM - 3:00 PM
Specialties
Discover Recent Posts
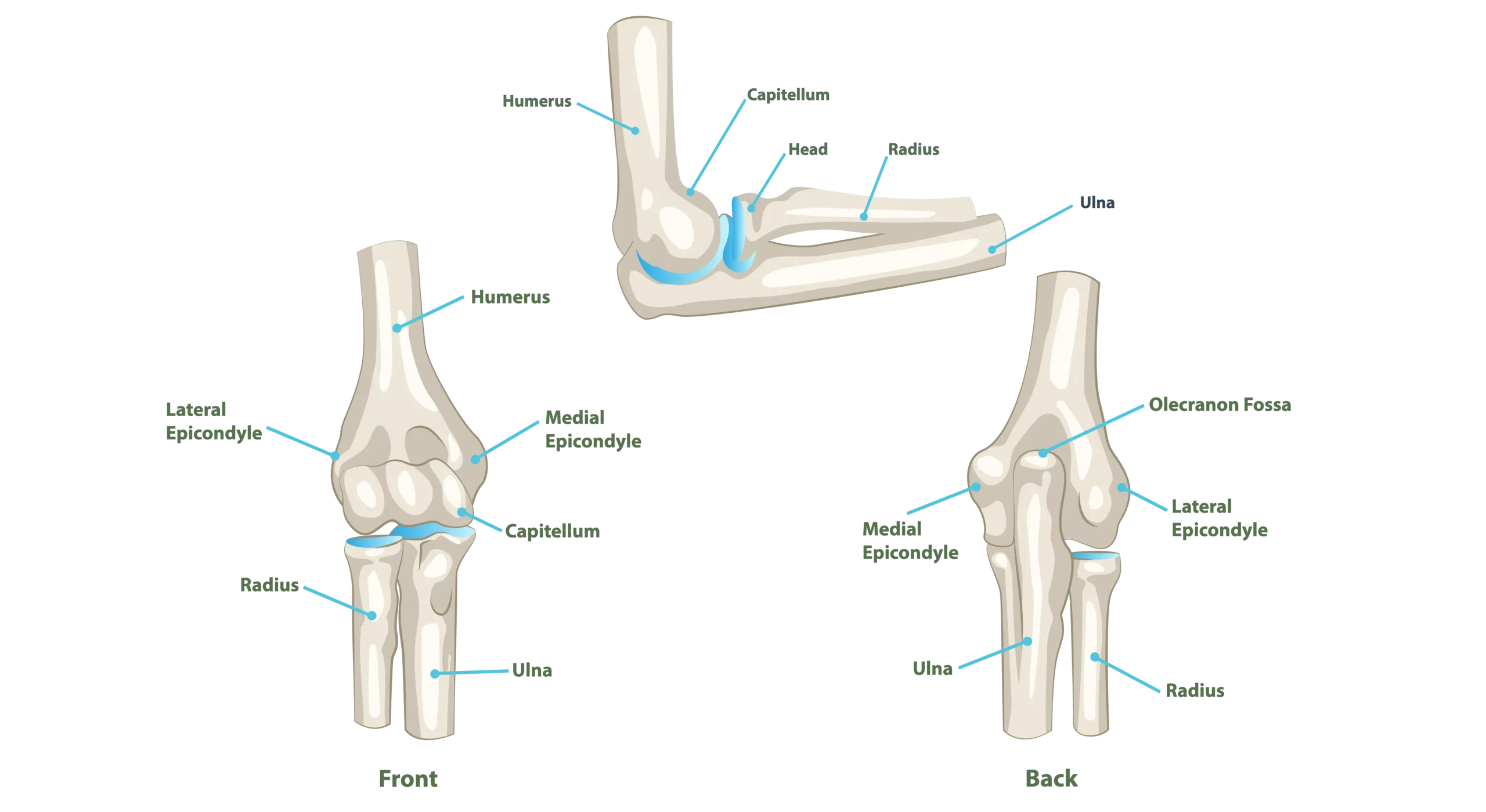
Elbow Anatomy
The elbow is made up of three main bones: the upper arm bone (humerus) and the two forearm bones (radius and ulna). Its primary function is to allow the arm to bend, straighten, and rotate the forearm and hand. As both a hinge and pivot joint, the elbow supports movements used throughout daily life.
This joint allows for actions such as lifting, reaching, throwing, turning a doorknob, typing, or carrying objects. These motions are essential for work, self-care, and recreational activities.
However, the structure that allows for such versatility also makes the elbow vulnerable to issues like overuse injuries, ligament tears, fractures, and arthritis.
Dr. Diaz provides focused, personalized care for elbow conditions. During your consultation, she will work to identify the source of your symptoms and create a treatment plan that considers your activity level, functional needs, the condition of your elbow, and your overall health.
Specific Elbow Conditions
Distal Biceps Tendon Rupture
The biceps muscle, which runs from the shoulder to the forearm, plays a critical role in bending the elbow and rotating the forearm (turning the palm up). At the elbow, the distal biceps tendon attaches the muscle to the forearm bone.
When this tendon tears, often during a forceful lift or when the elbow is forcibly straightened, patients typically experience a sudden, sharp pain. This pain may be accompanied by swelling, bruising, and a visible bulge where the muscle retracts. Many report hearing a “pop” at the moment of injury.
Distal biceps tendon ruptures most commonly occur in men between ages 40 and 60 and generally require surgical repair within six weeks of injury. Delayed treatment can make repair more difficult and less effective.
The repair surgery typically involves making an incision over the tendon’s insertion point, retrieving the tendon, and anchoring it back to bone with a surgical implant. After surgery, a hinged brace is used to protect the repair, and patients should avoid lifting and palm-up forearm rotation for several weeks.
Physical therapy typically begins around 12 weeks post-op. Most patients regain full strength and function by 5–6 months, though risks such as stiffness or nerve irritation can occur. With timely treatment, outcomes are overwhelmingly positive.
Tennis Elbow (Lateral Epicondylitis)
Tennis elbow is a degenerative condition involving the tendons on the outer side of the elbow that extend the wrist and fingers. It’s often caused by repetitive gripping, lifting, or twisting motions, and is common in athletes, office workers, and weightlifters.
Symptoms include burning or aching pain along the outside of the elbow, especially when lifting objects, shaking hands, or typing. Grip strength may also be reduced.
Initial treatment focuses on activity modification, rest, bracing, anti-inflammatory medications, and physical therapy. In some cases, injections such as platelet-rich plasma (PRP) or corticosteroids may provide relief. Surgical treatment may be considered for persistent symptoms that fail to improve after six months of nonoperative care.
Golfer’s Elbow (Medial Epicondylitis)
Golfer’s elbow affects the tendons on the inside of the elbow responsible for wrist flexion and gripping. It’s caused by repetitive stress and overuse, commonly seen in golfers, throwers, weightlifters, and those with repetitive manual tasks.
Patients typically experience aching pain along the inner elbow, pain with gripping or lifting (especially with the palm facing down), and tenderness when pressure is applied over the medial epicondyle.
Non-surgical treatment includes rest, activity modification, anti-inflammatories, forearm strengthening, and physical therapy. Elbow braces or splints may help relieve pressure on the tendons. If symptoms persist despite these measures, surgical debridement and tendon repair may be considered.
Elbow Arthritis
Arthritis of the elbow can result from age-related wear and tear (osteoarthritis), previous trauma, or inflammatory conditions such as rheumatoid arthritis. Over time, the smooth cartilage that lines the joint wears away, causing pain, stiffness, and reduced range of motion.
Common symptoms include pain with movement, joint swelling, mechanical catching or locking, and difficulty with everyday tasks like lifting, reaching, or straightening the elbow.
Treatment typically begins with activity modification, NSAIDs, corticosteroid injections, and physical therapy to preserve motion and function. In more severe cases, surgical options include arthroscopic debridement, osteophyte (bone spur) removal, or joint replacement depending on the degree of damage and the patient’s activity level. Some patients may require total elbow arthroplasty, particularly if joint destruction is advanced.
Ulnar Nerve Compression (Cubital Tunnel Syndrome)
Cubital tunnel syndrome occurs when the ulnar nerve becomes compressed or stretched at the inside of the elbow, where it passes behind the medial epicondyle. This is the same area known colloquially as the “funny bone.”
Early symptoms include numbness and tingling in the ring and pinky fingers, especially at night or when bending the elbow. As the condition progresses, patients may notice weakness in the hand and difficulty gripping.
Initial treatment includes activity changes (avoiding prolonged elbow bending), use of a nighttime elbow splint, and anti-inflammatory strategies. If nerve compression persists or causes functional loss, surgical release or repositioning of the nerve may be needed to prevent permanent damage.
Elbow Fractures
Fractures involving the bones around the elbow can occur from falls, direct trauma, or high-impact accidents. Symptoms include immediate pain, swelling, deformity, bruising, and an inability to move the elbow.
Some simple, non-displaced fractures can heal with immobilization in a splint or sling, along with ice and oral pain relief. However, more complex or displaced fractures may require surgery to realign the bones and stabilize them with plates, screws, or pins.
Recovery varies based on the type and severity of the fracture but generally involves a period of immobilization followed by progressive rehabilitation to restore motion and strength.
Olecranon Bursitis
Olecranon bursitis is inflammation of the small fluid-filled sac (bursa) located at the tip of the elbow. The bursa normally cushions the bone and skin, but when irritated or inflamed, it can fill with excess fluid and become swollen and painful.
This condition can result from repetitive pressure (like leaning on the elbows), trauma (such as a fall or bump), infection, or medical conditions like gout or rheumatoid arthritis. Patients often notice a soft, golf ball-sized swelling over the back of the elbow that may or may not be painful.
Treatment depends on the cause. Non-infectious bursitis often responds to rest, compression, NSAIDs, and avoidance of aggravating activities. If the swelling is significant, aspiration (draining the fluid) may be performed.
Infected bursitis requires antibiotics, and sometimes surgical drainage. For recurrent or chronic cases, bursectomy (surgical removal of the bursa) may be considered.
Elbow Instability
Elbow instability occurs when the joint becomes loose or prone to partial dislocation (subluxation) or complete dislocation. This condition may result from trauma, such as a fall or elbow dislocation, or from repetitive stress that stretches or damages the supporting ligaments.
Patients with instability often describe a feeling of the elbow “giving way” during pushing movements or athletic activities. Pain, clicking, or catching with motion may also occur. Athletes involved in overhead or throwing sports, such as baseball pitchers or gymnasts, are especially at risk.
Diagnosis involves a thorough clinical exam and imaging studies, such as X-rays or MRI. Mild cases may improve with bracing and targeted strengthening of the muscles around the elbow. More severe instability, or cases involving torn ligaments, may require surgical reconstruction to restore joint stability and function. Recovery from elbow stabilization surgery includes a period of immobilization followed by a structured rehab program to regain strength and motion.
Treatment & Recovery
Elbow treatment is most effective when tailored to a patient’s individual symptoms, lifestyle, and activity demands. Dr. Diaz provides personalized, evidence-based care for elbow injuries with a focus on restoring strength, motion, and long-term joint health.
Non-Surgical Treatments
Conservative care is often the first step and may include:
Oral or injectable anti-inflammatories
Activity modification or rest
Immobilization with a brace or sling
Physical therapy to restore strength and mobility
Ice, compression, and ergonomic adjustments for daily tasks
Surgical Treatments
When non-operative care fails to resolve symptoms, or in cases of severe injury, Dr. Diaz offers minimally invasive and advanced surgical solutions, including:
Tendon repairs (e.g., distal biceps rupture)
Ligament reconstruction for instability
Elbow fracture fixation
Removal of inflamed bursae (bursectomy)
Ulnar nerve decompression or transposition
Arthroscopy for loose bodies or cartilage issues
Rehabilitation and Recovery
Recovery plans are customized to your procedure and personal goals. These typically involve:
A guided return to motion using a staged protocol
Physical therapy when appropriate to regain flexibility and strength
Home exercise programs to prevent stiffness and optimize healing
Gradual return to sports, work, or overhead activities
Most patients can expect steady improvement in function and pain relief with the right treatment plan. Dr. Diaz partners closely with each patient throughout the healing process to ensure optimal recovery and safe return to the activities that matter most.


